The problem
IL-1 Effects:

IL-1α and IL-1β are both important in cancer development

High IL-1 expression in cancer confers poor prognosis

Overexpression of interleukin-1β induces gastric inflammation and cancer and mobilizes myeloid-derived suppressor cells in mice



IL-1β mAb reduces G-MDSC and KC (IL-8) in mouse kidney cancer (RCC) model

Combination of anti–IL-1β with anti–PD-1 or cabozantinib treatment improves the outcome of RCC in mice
Combination of anti–IL-1β with anti–PD-1 treatment improves the outcome of 4T1 mammary carcinoma in mice

The Solution
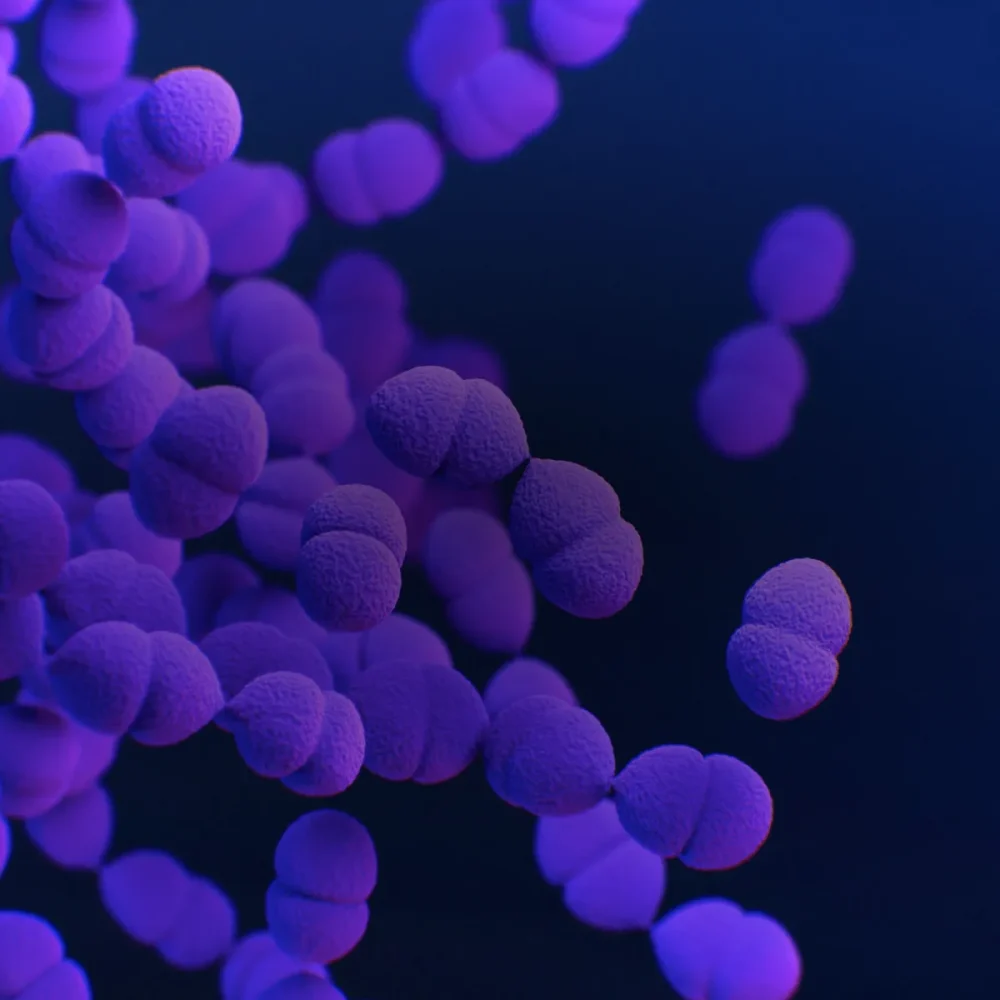
Isunakinra – a very potent IL-1 blocker

Isunakinra binds IL1R1 with high affinity and blocks the binding of the natural agonists: IL1α and IL1β
“CRP, IL-6 and IL-8 are prognostic factors for checkpoint inhibition”

Isunakinra – is being tested in a clinical phase I/II trial in solid tumor patients – combining with a PD-1 inhibitor
Step by step
How does it work?
We do this
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
We do this
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
We do this
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
We do this
Lorem ipsum dolor sit amet, consectetur adipiscing elit.

Words from our Board of Directors
At Buzzard Pharmaceuticals, we are not just developing medicines — we are redefining hope for patients worldwide. Our team’s dedication and innovative spirit reflect our commitment to bringing safe, life-changing therapies to those who need them most.
Carl-Johan Spak
Board member, Buzzard Pharmaceuticals